Abdominal surgery such as laparotomy, stoma closure and incisional hernia repair could carry a high rate of surgical site complications (SSCs).8-13
Challenge the norm
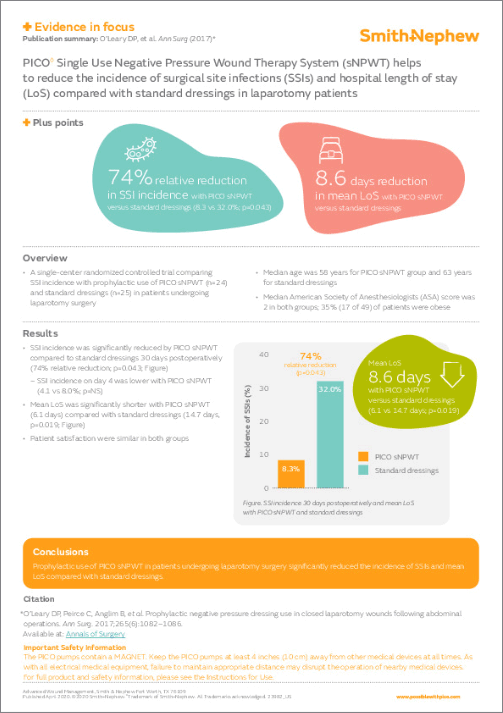
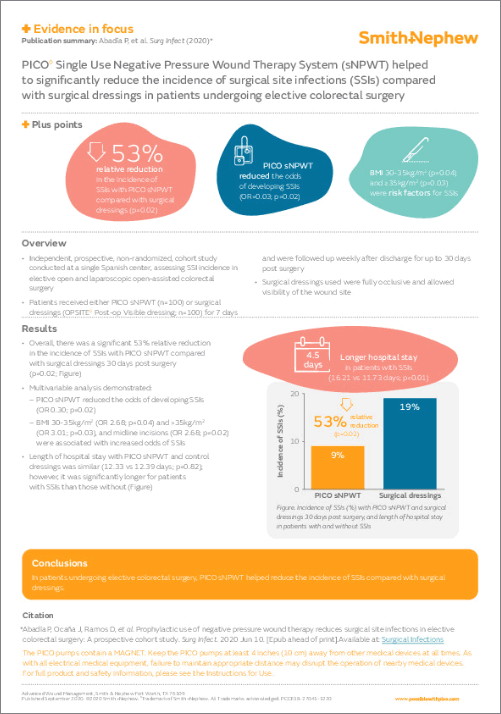
Following abdominal surgery, PICO sNPWT has been shown to significantly reduce:*
- Incidence of SSCs, including SSIs1-3,5-7
- Length of stay (LoS)2,4-6
- Readmission rates5
General, colorectal, vascular surgery
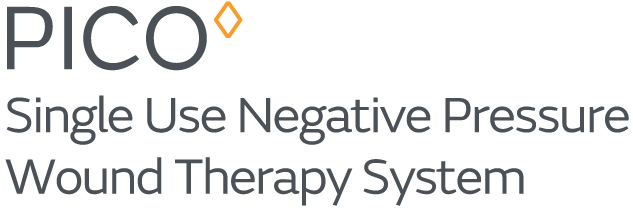
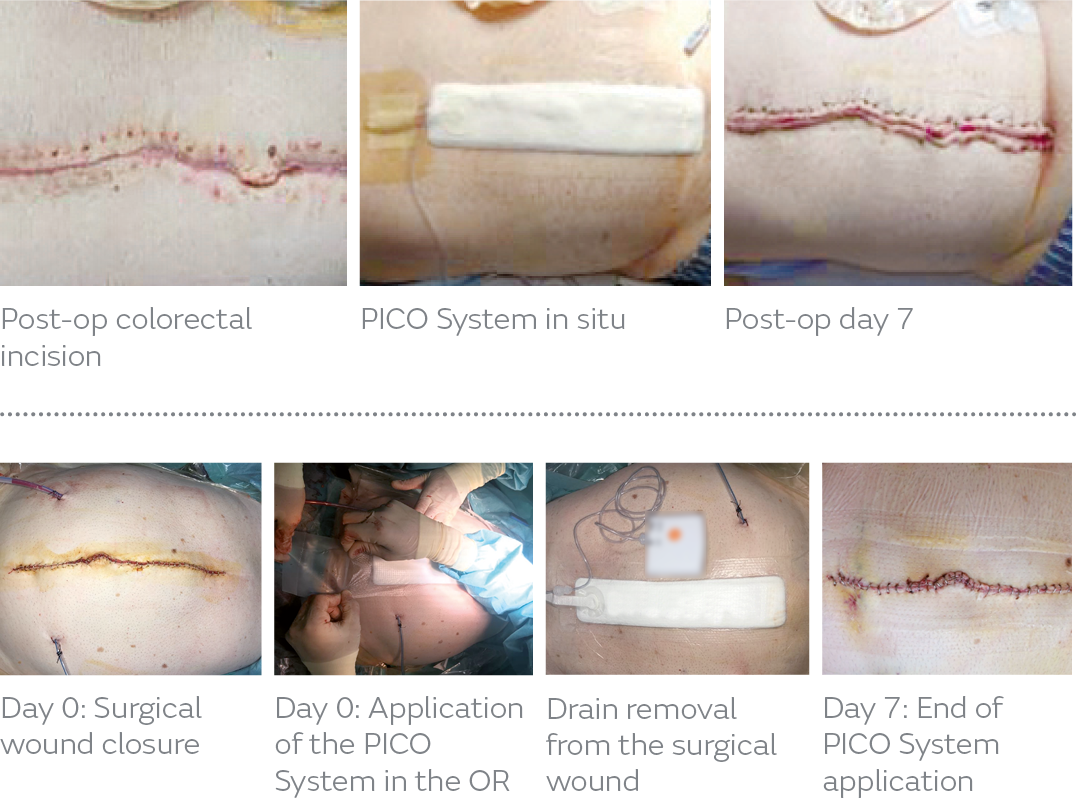
Application tips
- The PICO 7 or PICO 14 System may be appropriate for these procedures
- The PICO System may be used in conjunction with surgical drains provided the dressing is not placed over tubing where it exits the skin
- Exudation: low/moderate
- Remove excess hair and use NO STING SKIN-PREP◊ Skin Protectant if needed
- For wounds 0.5cm–4.5cm deep, a filler may be required
- Fillers: ACTICOAT◊ FLEX Dressing, foam, gauze
- Do not place gauze into blind or unexplored tunnels
- Do not use over exposed arteries, veins, nerves or organs
- Port position: uppermost from incision
- In areas of complexity, fixation strips or gel strips* (*not included in kit) may be used to maintain a seal
- Dressing may be left in place for up to 7 days. The PICO 14 Pump will continue therapy for 14 days.
- Gupta R, Darby GC, Imagawa DK. Efficacy of negative pressure wound treatment in preventing surgical site infections after whipple procedures. Am Surg. 2017;83(10):1166–1169.
- O'Leary DP, Peirce C, et al. Prophylactic negative pressure dressing use in closed laparotomy wounds following abdominal operations: a randomized, controlled, open-label trial: The P.I.C.O. Trial. Ann Surg. 2017;265:1082–1086.
- Abadía P, Ocaña J, Ramos D, et al. Prophylactic use of negative pressure wound therapy reduces surgical site infections in elective colorectal surgery: A prospective cohort study. Surg Infect. 2020 Jun 10. [Epub ahead of print].
- Obeid N, Sharma E, Dunstan M, et al. Negative pressure therapy for stoma closure sited – a nonrandomised case control study. Int J Colorectal Dis. 2020 Sep 14;[Epub ahead of print].
- Selvaggi F, et al. New advances in NPWT for surgical wounds of patients affected with Crohn’s disease. Surg Technol Int. 2014;24:83–89.
- Interim data: Pellino G, et al. Effects of a new pocket device for NPWT on surgical wounds of patients affected with Crohn’s disease: a pilot trial. Surg Innov. 2014;21(2):204–212.
- Bueno-Lledó J, Franco-Bernal A, Garcia-Voz-Mediano MT, Torregrosa-Gallud A, Bonafé S. Prophylactic Single-use Negative Pressure Dressing in Closed Surgical Wounds After Incisional Hernia Repair: A Randomized, Controlled Trial. Annals of Surgery. 2020 Nov 12.
- Tanner J, Khan D, Aplin C, Ball J, Thomas M, Bankart J. Post-discharge surveillance to identify colorectal surgical site infection rates and related costs. Journal of Hospital Infection. 2009 Jul 1;72(3):243–50.
- Petrosillo N, Drapeau CM, Nicastri E, Martini L, Ippolito G, Moro ML. Surgical site infections in Italian hospitals: a prospective multicenter study. BMC Infectious Diseases. 2008 Dec 1;8(1):34.
- Wick EC, Gibbs L, Indorf LA, Varma MG, Garcia-Aguilar J. Implementation of quality measures to reduce surgical site infection in colorectal patients. Diseases of the colon & rectum. 2008 Jul 1;51(7):1004–9.
- Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG, Foley EF. Wound infection after elective colorectal resection. Annals of surgery. 2004 May;239(5):599.
- Yoshida J, Shinohara M, Ishikawa M, Matsuo K. Surgical site infection in general and thoracic surgery: surveillance of 2 663 cases in a Japanese teaching hospital. Surgery Today. 2006 Feb 1;36(2):114–8.
- Serra-Aracil X, Espin-Basany E, Biondo S, Guirao X, Orrego C, Sitges-Serra A. Surgical site infection in elective operations for colorectal cancer after the application of preventive measures. Archives of surgery. 2011 May 1;146(5):606–12.
* Compared with standard surgical dressings; n = 25 vs n = 36; p = 0.01
† Compared with standard surgical dressings; n = 24 vs n = 25; p = 0.043
‡ Compared with standard surgical dressings; n = 24 vs n = 25; p = 0.019
§ Compared with traditional packing; n = 17 vs n = 15; 5 vs 6 days
Π Compared with traditional packing; n = 17 vs n = 15; 1.9 vs 11.9 visits
¶ Compared with standard surgical dressings; n = 25 vs n = 25; p = 0.008
# Compared with standard surgical dressings; n = 24 vs n = 25; p = 0.019
Δ Compared with standard surgical dressings; n = 72 vs n = 74; 16.6 v 29.8%; p < 0.042
Ω Compared with standard surgical dressings; n = 72 vs n = 74; 0 vs 8%; p < 0.002